A Guide to Recognizing Depression in Older Adults
Disclaimer: If you or your loved one is showing signs of depression and suicide ideation, dial “988” or contact the 988 Suicide & Crisis Lifeline.
Everyone feels down now and then. But while the occasional bad day is normal, depression is not, and yet it impacts millions of people in the U.S.
According to the National Institute on Aging, depression is a serious mood disorder that can affect the way an individual feels, thinks, and acts—with roughly 2 million of the 34 million Americans aged 65 and older experiencing some form of depression. While depression is a prevalent issue, it is treatable.
Knowing when your loved one is experiencing depression can be tough to figure out. Not everyone wants to share that information, or they may think it’s just a part of growing old. However, it’s a serious, life-altering issue.
“Most people often mistake memory loss, sadness, anxiety, or worry as just part of getting older. But the aging experience does not involve these experiences as part of a normal trajectory. Older adults who live with these issues think it’s just part of life, when really, it’s a treatable mental health issue,” said Deborah Serani, a psychologist and professor at Adelphi University in New York and author of Depression in Later Life: An Essential Guide.
“Late-life depression is a critical problem, and many older adults may not seek treatment,” said Ellen Lee, assistant professor of psychiatry and division chief of geriatric psychiatry at the University of California, San Diego (UCSD), and a staff psychiatrist at the VA San Diego Healthcare System.
According to the World Health Organization, the older population is aging quickly. By 2050, the world population over age 60 is expected to almost double from 900 million in 2015 to 2 billion. Approximately 15% of older adults suffer from a mental disorder. Mental health problems are under-identified by health care professionals, yet due to the stigma surrounding the conditions, many older adults may be reluctant to get help.
What Are the Risks?
The Centers for Disease Control and Prevention (CDC) reported that older adults are at an increased risk of depression. This is because 80% have at least one chronic health condition, and 50% have two or more illnesses such as cancer or heart disease, which can limit your ability to function. Also, according to the federal report Older Americans 2020: Key Indicators of Well-Being, 13% of women aged 65 and older reported more clinically relevant depressive symptoms compared with 9% of older men.
The National Institutes of Mental Health (NIMH) reports that depression can be diagnosed at any age. Older adults may also be at a higher risk of developing depression if they:
- Are lonely or socially isolated
- Are female
- Have a disability
- Sleep poorly
- Take certain medications
- Have personal or family history of depression
- Are experiencing stress stemming from a life event, such as a divorce or loss of a spouse
Why the Stigma?
“The most classic symptom of depression is feeling sad for most of the day for two weeks,” said Mark Kunik, a geriatric psychiatrist and professor in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine in Houston and a physician at the Michael E. DeBakey VA Medical Center.
“However, compared to younger adults, older adults are less likely to vocalize that they’re depressed and instead will speak about related physical ailments such as ‘feeling tired’ or ‘having no energy’ and they’re not vocalizing their sadness because they’re ashamed. They think mental health is a character flaw or a marker of weakness of mind and body. In addition, prior to the 1960s there were little scientifically proven psychiatric treatments,” said Dr. Kunik. “Older adults are less likely to see mental illness as biological as heart disease or hypertension. They see it as something in their control and their fault.”
Getting older is an experience that our modern society tends to devalue, added Dr. Serani. “When it comes to mental illness, the public fears and distances themselves from individuals who have a mental health disorder. So, when older adults begin to struggle with a mental health issue, they must deal with the double burden: ageism and mental illness stigma. This is why it’s hard to talk about mental illness with older adults. No one wants to feel different, singled out, or seen as vulnerable by being older or by having a mental illness.”
As people age, there is increased risk for certain mental health problems. When an older adult has cognitive decline or dementia, they are likely to have depressive symptoms, said Dr. Lee. “Seeking mental health care for the first time as an older adult may be challenging for many individuals. They may feel uneasy speaking to their primary care doctors about these problems and have limited knowledge about the different treatments.”
Yet, despite how common depression is, it may not be discussed much by an individual and their doctor, which means that you may want to bring it up and help advocate for your loved one. A study in the Journal of the American Geriatrics Society found that primary care doctors spend little time discussing mental health care with older adult patients.
Signs of Depression
Having healthy social relationships is a key element needed for humans to thrive, and a lack of connection paired with social isolation, or experiencing the death of a loved one, can cause anyone to go into a depression, but particularly vulnerable are adults over age 70.
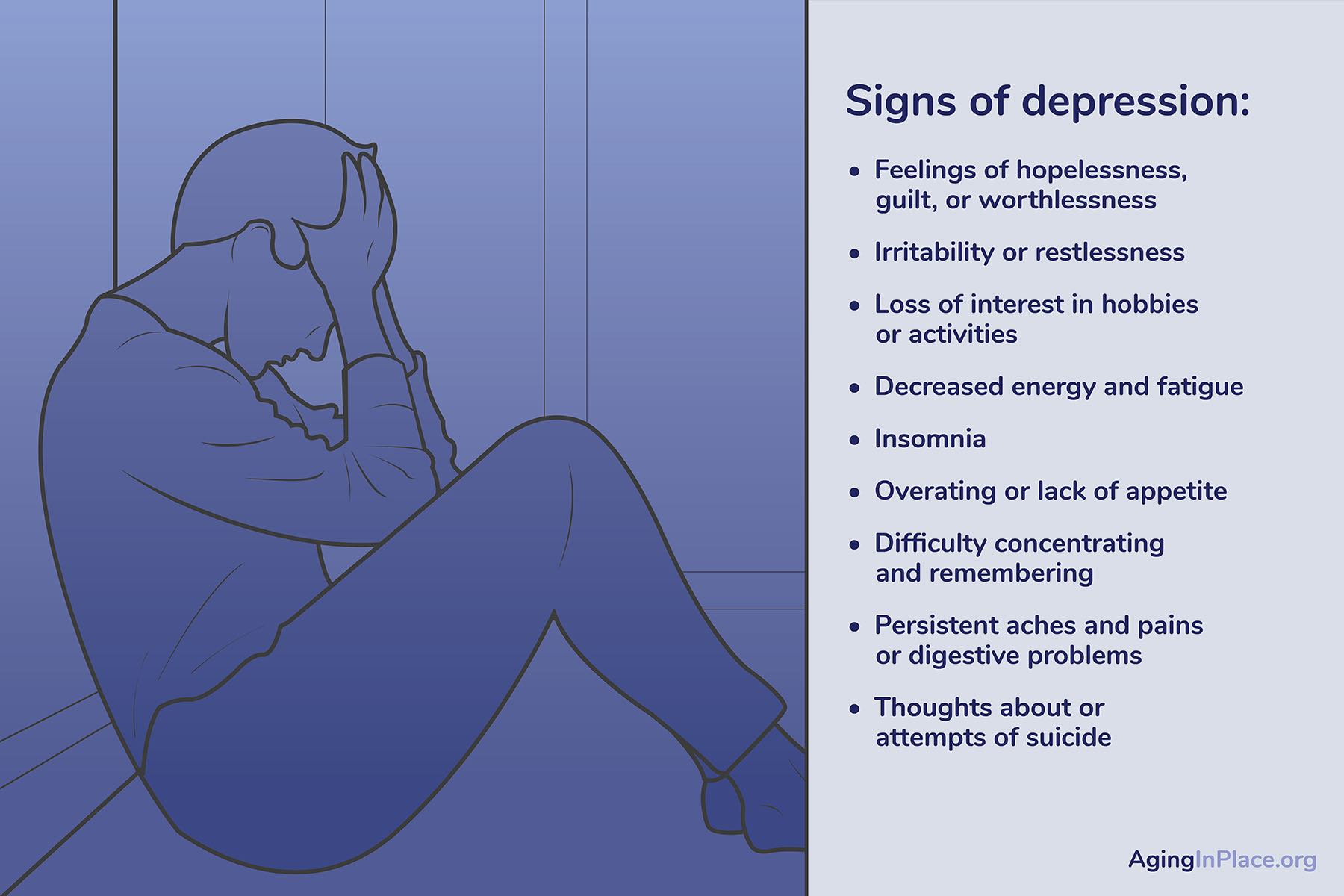
Other symptoms to look for that indicate an individual is dealing with depression, according to the CDC, may include:
- Feelings of hopelessness, guilt, worthlessness
- Irritability, restlessness
- Loss of interest in hobbies or activities
- Decreased energy and fatigue
- Insomnia
- Overeating or lack of appetite
- Difficulty concentrating and remembering
- Persistent aches and pains or digestive problems
- Thoughts about or attempts of suicide
“There are validated measures available to help screen for suicidality,” noted Lauren Masopust, a licensed marriage and family therapist who provides psychotherapy to youths, adults, couples, and families. “These screeners, such as the (C-SSRS), the Columbia-Suicide Severity Rating Scale, are available in many primary care providers’ offices.”
According to the American Psychological Association, suicidal ideation behaviors to be on alert for include:
- Talking about committing suicide
- Trouble eating or sleeping
- Changes in behavior
- Social withdrawal
- Lack of interest in hobbies and school
- Previous attempts at suicide
- Experienced recent losses
- No longer cares about personal appearance
For the full list, visit the American Psychological Association.
“If an older adult is expressing suicidal thoughts or talking about harming themselves, it’s important to connect them to help as soon as possible,” said Dr. Lee. “Resources such as the new Suicide and Crisis lifeline (988) or the local emergency room are critical in those situations.”
Benefits of Addressing Mental Health
Talking about mental health can allow you to move forward and start finding solutions, as well as help improve relationships that may be strained.
“Family and friend support is one of the most important ingredients for preventing and treating depression and other mental health problems,” said Dr. Kunik.
“If older adults are willing to talk about some of these problems, the social support can have a huge impact. Loved ones can help validate that these symptoms are important and may be indicative of a mental health problem. Older adults may feel reassured that these symptoms are linked to a treatable problem, rather than perceiving it as a personal failure or fault. They may also benefit by having their loved ones accompany them to appointments,” said Dr. Lee. “When older adults talk about mental health struggles with their loved ones, it opens the door for others to share their experiences. Being approachable about mental health is an important way to fight the stigma.”
It’s also helpful to be a role model by talking about your own experiences with balancing a sense of mental health. “If you’ve been in psychotherapy or take medication for a mental health issue, share stories about its positive impact on your life,” said Dr. Serani. “Help your loved one understand that good health includes not just physical wellness but mental wellness too.”
How to Start the Conversation
If you’re a caregiver with a depressed patient, or see a loved one who is struggling with symptoms, you may want to set the scene for a low-pressure talk about it. This could involve going outside for a walk or simply making sure no one else is in the room. Privacy is important. Even if you’re afraid to touch upon a sensitive topic, do take that next step. You can help start the dialog and let your loved one know that you care, and that you’re there for them.
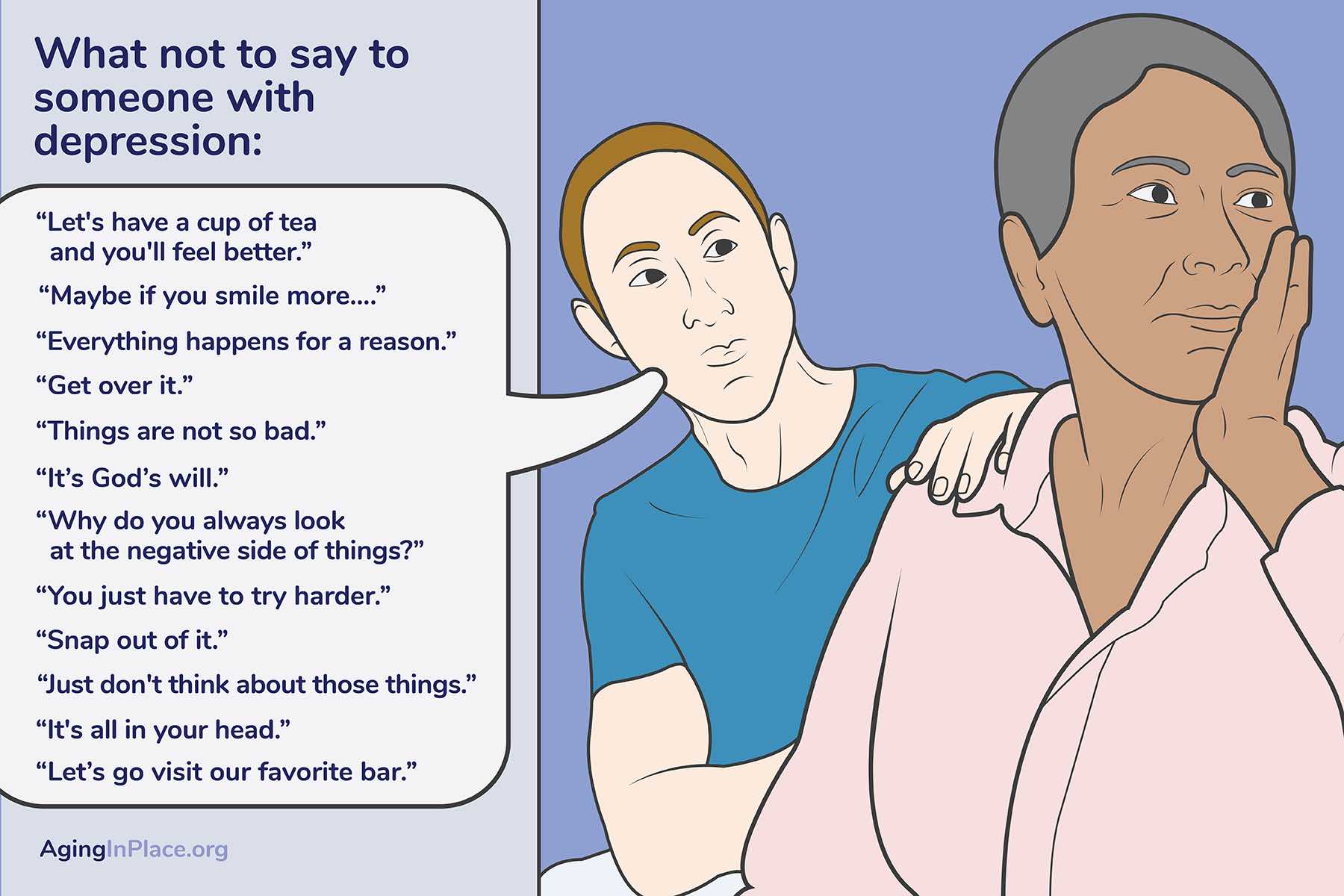
“It’s impossible to always say the right thing. Being genuine, present, and caring, while acknowledging if your loved one is upset by what you said, is often a good approach,” said Dr. Lee. “Comments such as ‘You’ll be fine’ or ‘You just need to snap out of it,’ could sound dismissive and make older adults feel less comfortable sharing. When I work with patients, I try to use their language and words to describe symptoms and try to avoid placing my own labels on their problems. Some patients respond better if I say, ‘Could you tell me some more about your low motivation?’ rather than, ‘Is your low motivation because of your depression?’”
Ask how they are doing and really listen, added Dr. Kunik. You can try saying: “You don’t seem your usual self, share with me what is going on.” Or, “Sometimes, it helps to talk to family or a friend, let’s take some time now to talk through what is upsetting you.” Sometimes a walk or a drive can make for an easier conversation about difficult issues.
What Not To Say
You want to make sure you’re not minimizing or shaming your loved one with your words, as that can deepen feelings of stigma, noted Dr. Serani. For example, she advised caregivers and loved ones to refrain from using phrases that could seem flippant, like: “This too shall pass” or “You’re just too sensitive.”
It’s also important to avoid toxic positivity—an overly positive approach—such as, “You have so much to be happy about,” because that denies another’s true experiences, added Dr. Serani. “While many people believe a positive approach can encourage others, if it’s too intense or too prevalent, it can be devaluing and critical.”
Solutions and Treatment
According to the National Institute on Aging, although most cases of depression can’t be prevented, making some healthy lifestyle changes can benefit your mental health. The first step is to take your loved one to get a physical medical exam.
“Once you know your older adult is in good physical health, make an appointment with a geriatric mental health professional. With specialized training in gerontology, they can help assess your loved one’s mental and emotional health,” said Dr. Serani. “Working with a health professional who understands geriatric or older adult issues helps because they have specialized training in the aging cycle and chronic conditions seen in later life. Just like you would take your children to a pediatrician, a specialist who understands child development and growth, seeing a health professional with geriatric training will get you the best treatment for this age group. You can find these specialists in your community or through your local hospital,”
She continued: “If a diagnosis for a mental health disorder occurs, make sure to be a part of your loved one’s health team. Ask your loved one to sign off on your ability to share and obtain information. Or if your loved one is very ill, seek power of attorney so you can lead their care in an active manner. Take time to learn about their mental health disorder. Read. Join a mental health awareness group or take a seminar. By doing so, you become an advocate for your loved one.”
There are also innovative treatments for mental health, as well as new developments on the horizon, noted Dr. Lee. “The two mainstays of psychiatric treatments are medications (such as antidepressants) and psychotherapy (or talk therapy). Studies have shown that combining both medication and psychotherapy treatments result in better outcomes for depression than either medication or psychotherapy alone. In fact, the combination of therapies has a synergistic effect, i.e., an effect that is greater than the sum of each component,” she said.
A newer treatment approach is neuromodulation—stimulating the brain directly through electroconvulsive treatment or repetitive transcranial magnetic stimulation—which Dr. Lee explained has “been shown to be effective for a number of mental health issues including depression.” The FDA approved transcranial magnetic stimulation (TMS) for medication-resistant depression in 2008. Medically necessary treatments are covered by many insurance companies.
Prevention
According to Dr. Kunik, doing certain activities, such as walking 20–30 minutes a day, volunteering, attending religious services, or communicating regularly with friends and family, can help prevent depression. Also, try spending no more than an hour a day watching the news or following politics on social media.
Geriatric depression does not have to slow you or your loved one down. With a proper diagnosis and targeted treatment, people can improve their well-being and physical health, said Dr. Serani. “The golden years can remain a meaningful chapter in your loved one’s life.”
WRITTEN BY
An experienced journalist and content writer, Julie Weingarden Dubin specializes in mental health, medicine, wellness, health and science. Dubin’s credits include Prevention, Newsweek, Time, WebMD, HealthCentral, Psycom, Well+Good, Health Monitor Network, Forbes, Arthritis Today, Reader's Digest, SELF, Psychology Today, Marie Claire, Good Housekeeping, Better Homes and Gardens, Cosmopolitan, Woman’s Day, Parents, Parenting, American Baby, Fit Pregnancy, Shape, TODAY and MSNBC. Dubin’s freelanced for Johns Hopkins Children Center, Johns Hopkins Medicine, Baptist Health, Wolfson Children’s Hospital, Children’s Hospital of Michigan and HAP Balanced Living. Dubin received her journalism degree from the University of Wisconsin—Madison.
MEDICALLY REVIEWED BY

