Nothing is more important than breathing. It affects every aspect of your health and life. If you’re struggling to breathe and have been prescribed oxygen therapy, you’re probably wondering what your options are, what it will cost, and how you will pay for it.
Working through and understanding insurance coverage—especially Medicare coverage—can be a complicated, frustrating, and time-consuming task. Websites are full of conflicting and out-of-date information. We have put together a comprehensive, one-stop resource for those attempting to understand Medicare coverage of portable oxygen concentrators (POCs).
Benefits of a Portable Oxygen Concentrator vs. Oxygen Tanks
Older home oxygen delivery systems relied on compressed gas and liquid oxygen that are housed in tanks. These tanks were tricky to maneuver and take on trips because of their size and weight. They were difficult to travel with because you’d need multiple replacement tanks, and airlines don’t allow oxygen tanks because they contain hazardous materials and could explode.
The introduction of portable oxygen concentrators made travel and activities much more accessible to those reliant on supplemental oxygen. These machines are small and eliminate the need for tanks. They can be carried in small shoulder bags or backpacks. The only thing you have to worry about is keeping the battery charged.
Other benefits of POCs include:
- Small, quiet, and inconspicuous
- Do not require replacement tanks
- Are easy to use (no complicated equipment or controls)
- Are easy to travel with
- Can be used on commercial airline flights
- Can run from 2–16 hours on one rechargeable battery (depending on mode and how fast someone breathes)
- Are great for mental and physical well-being
Dr. Alan Lidskly, an internal medicine physician with Kaiser Permanente, noted that those of his patients who were able to procure portable oxygen concentrators are thrilled with the freedom that they provide and appreciate their ability to attend functions and activities that they might not otherwise be able to attend. “POCs have a true quality of life benefit to patients,” he said.
Does Medicare Cover Portable Oxygen Concentrators?
Medicare’s coverage of portable oxygen concentrators is complicated. First, you need to qualify for Medicare. You are generally eligible if you’re 65 years or older, of any age with a disability making you unable to work for at least one year, or of any age with a fatal condition including end-stage renal disease (permanent kidney failure requiring dialysis or a transplant). You can visit Medicare’s eligibility tool to determine if you qualify and your expected premium. Here’s the result of entering a 1956 birthdate:
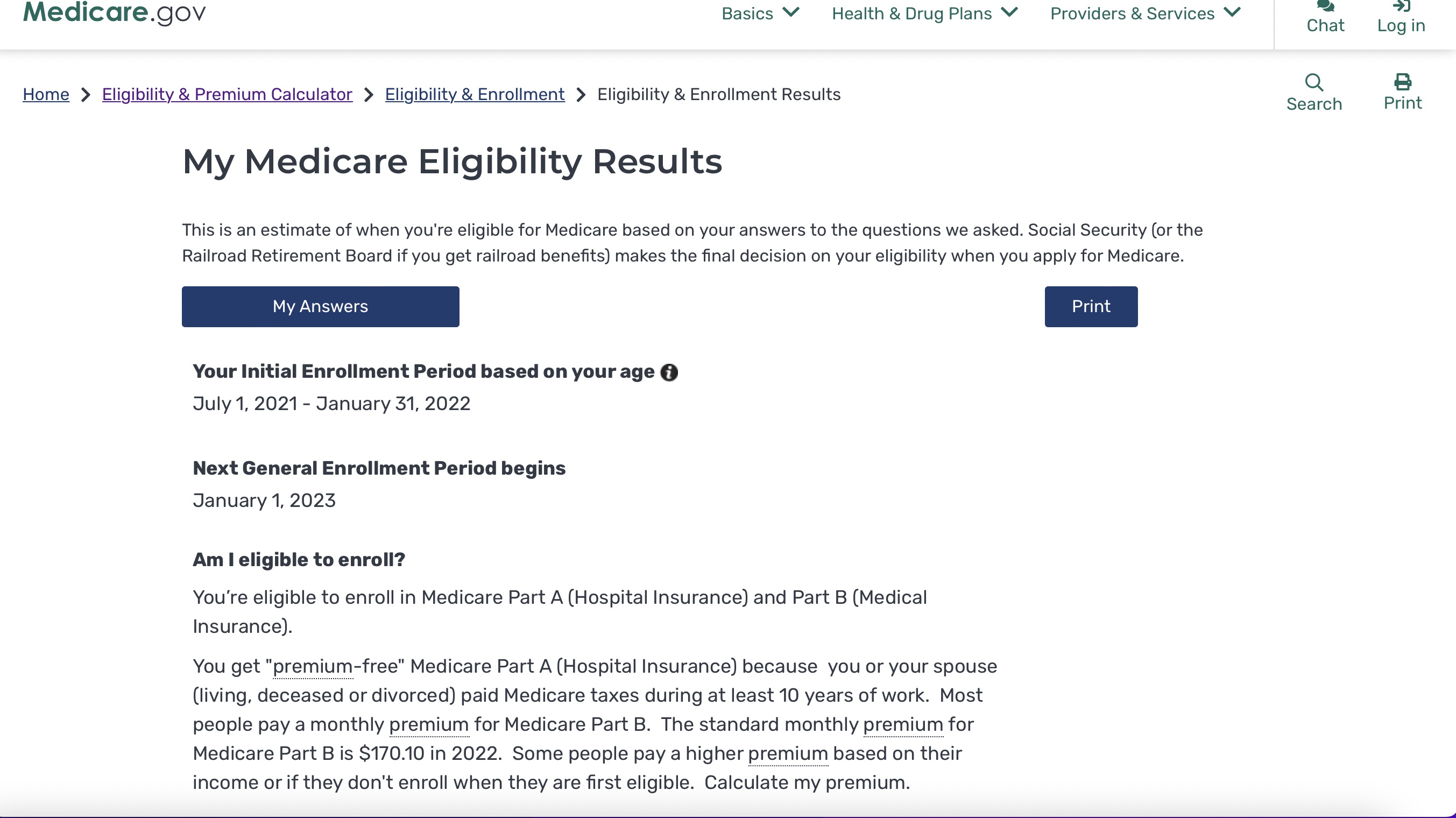
Medicare has two “parts”: Part A is hospital insurance and Part B is medical insurance. Part B covers durable medical equipment (DME) like oxygen equipment and accessories. For 2022, $170.10 is the standard monthly premium for Medicare Part B with a $233 yearly deductible. Medicare Advantage (sometimes called Part C) is provided by outside health insurance companies and includes Medicare Part A and B plus additional coverage. Premiums and deductibles vary by company.
Eligibility for Medicare Coverage of Oxygen Concentrators
POCs are covered under Medicare Part B as “durable medical equipment” (DME). Medicare defines DME as:
- Durable (can withstand repeated use)
- Used for a medical reason
- Not usually useful to someone who isn’t sick or injured
- Used in your home
- Has an expected lifetime of at least three years
Medicare explains its DME coverage as follows: “Part B covers DME when your doctor or other health care provider (like a nurse practitioner, physician assistant, or clinical nurse specialist) prescribes it for you to use in your home. A hospital or nursing home that’s providing you with Medicare-covered care can’t qualify as your ‘home’ in this situation. However, a long-term care facility can qualify as your home. If you’re in a skilled nursing facility (SNF) as part of a stay covered under Medicare Part A (Hospital Insurance), the facility is responsible for providing any DME you need while you’re in the facility for up to 100 days.”
A Certificate of Medical Necessity form must be provided to Medicare in order to commence home oxygen therapy.
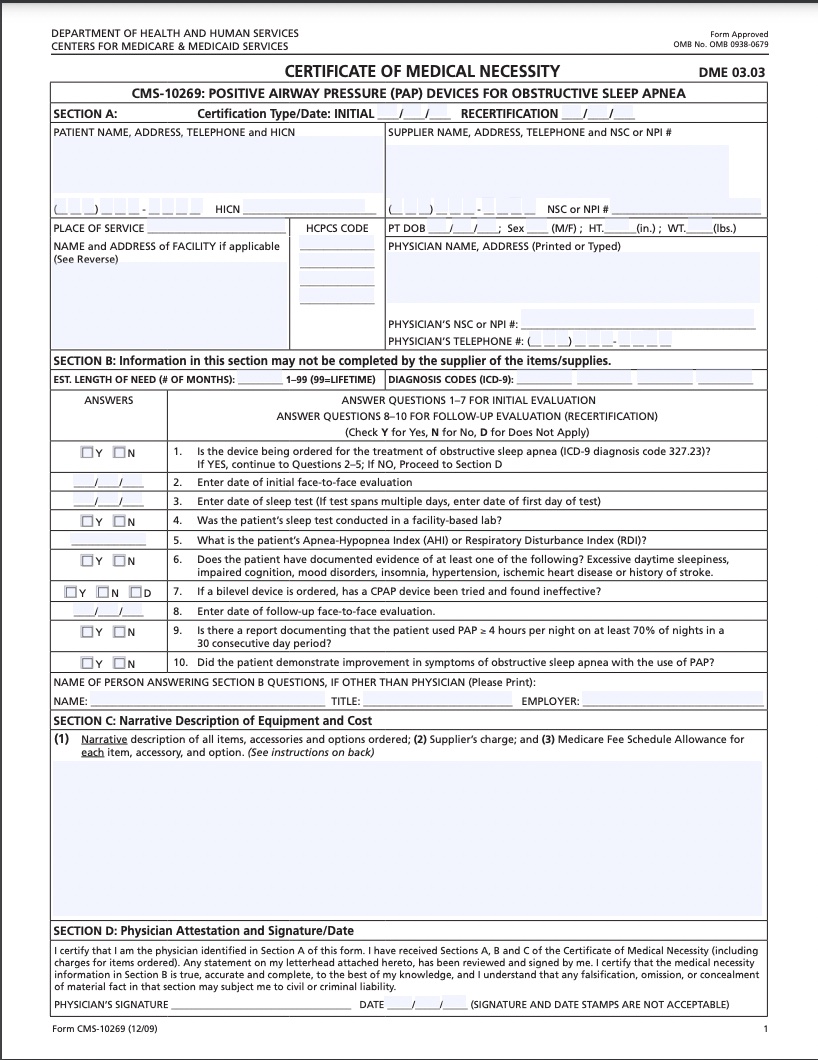
Suppliers must gather and supply the following information:
- Face-to-face evaluation documentation: You must have an in-person examination by a qualified medical professional capable of writing prescriptions (medical doctor, doctor of osteopathy, physician assistant, nurse practitioner, or clinical nurse specialist) within 30 days of the order date documenting the necessity of oxygen therapy. The report must include a respiratory diagnosis and state that the hypoxia-related symptoms may improve with oxygen therapy and document that alternative treatments (like medications or inhalers) have been considered or attempted and deemed ineffective.
- Arterial oxygen saturation testing documentation: A qualified medical professional must perform testing and document hypoxemia (low blood oxygen levels). They can measure blood oxygen levels with an ABG (arterial blood gas) test, which will give a number representing PO2 (partial pressure of oxygen) or they can use a pulse oximeter to measure oxygen saturation in the finger or on the ear. Testing must be performed while the patient is stable (not during severe illness or in an emergency room), within 30 days of certification, and the results documented in the patient’s medical records. Test results will put a patient in one of three categories:
- Group I (coverage limited to 12 months or shorter): If the patient is awake and at rest in room air and has a PO2 (amount of oxygen in the blood) of less than or equal to 55 mmHg (millimeters of mercury) or an oxygen saturation less than or equal to 88%, they qualify and no further testing is required. If these criteria are not met, exercise testing and/or sleep testing may be performed in order to demonstrate improvement in hypoxia.
- Group II (coverage limited to three months or shorter): Awake and at rest PO2 of 56–59 mmHg or oxygen saturation of 89% or less with a secondary diagnosis of:
- Dependent edema (swelling) suggesting congestive heart failure, or
- Pulmonary hypertension (high blood pressure in lungs) or cor pulmonale (enlarged heart due to high blood pressure in lungs), or
- Erythrocythemia (excessive red blood cell production) with a hematocrit (test measuring red blood cells) greater than 56%
- Group III (coverage denied): PO2 is greater than or equal to 60 mmHg or oxygen saturation is greater than or equal to 90%, regardless of the type of testing.
- Prescription by attending physician specifying:
- A diagnosis of the disease requiring home use of oxygen
- The oxygen flow rate
- An estimate of the frequency, duration of use, and duration of need
- The type of delivery system (compressed gas, liquid oxygen system, or oxygen concentrator)
Medicare may require periodic, continuing medical necessity reviews and repeat testing may be requested throughout the coverage period.
Coverage will likely be granted for patients with significant hypoxemia in the chronic stable state if the attending physician has determined that:
- The patient has a severe lung disease such as:
- Chronic obstructive pulmonary disease (COPD)
- Diffuse interstitial lung disease (a group of disorders affecting the connective tissues of the lungs)
- Cystic fibrosis
- Bronchiectasis (widened lung airways due to damage)
- Widespread pulmonary neoplasm (lung cancer)
- The patient has hypoxia-related symptoms or findings that might be expected to improve with oxygen therapy such as:
- Pulmonary hypertension (when the pressure in the blood vessels from the heart to the lungs is too high)
- Recurring congestive heart failure due to chronic cor pulmonale (enlarged heart due to high blood pressure)
- Erythrocytosis (increased production of red blood cells)
- Impairment of the cognitive process (trouble thinking, learning, remembering, and making decisions)
- Nocturnal restlessness (inability to stay asleep)
- Morning headache
All of the above pertains to oxygen systems in general but what about portable oxygen systems specifically? According to the Centers for Medicare and Medicaid Services, a portable oxygen system is usually covered if, in addition to the above requirements, “the medical documentation indicates that the patient is mobile in the home and would benefit from the use of a portable oxygen system in the home. Portable oxygen systems are not covered for patients who qualify for oxygen solely based on blood gas studies conducted during sleep.”
What is Your Cost for an Oxygen Concentrator?
Assuming you qualify, Medicare may cover part, but not all, of the cost of renting a portable oxygen concentrator. They do not cover purchase costs. Medicare’s coverage of oxygen equipment and accessories is as follows: If you have original Medicare (not Medicare Advantage), you’ll pay 20% of the Medicare-approved amount after meeting your Part B deductible. A deductible is a set amount designated by an insurance company that the policyholder must pay before the insurance company begins paying any claims. Medicare’s Part B deductible for 2022 year is $233. So, assuming you’ve met your deductible for the year, if your DME supplier agrees to rent out a POC for $200 per month, your cost would be 20% of that or $40 per month. A Medicare Advantage plan may pay an even higher proportion of the rental cost, leaving you with a smaller monthly payment.
A DME supplier negotiates a five-year rental contract with Medicare. The initial contract is for 36 months. If your doctor determines that you still need oxygen supplementation after that, the supplier is obligated to provide equipment and supplies to you under that contract for an additional 24 months (for a total of five years).
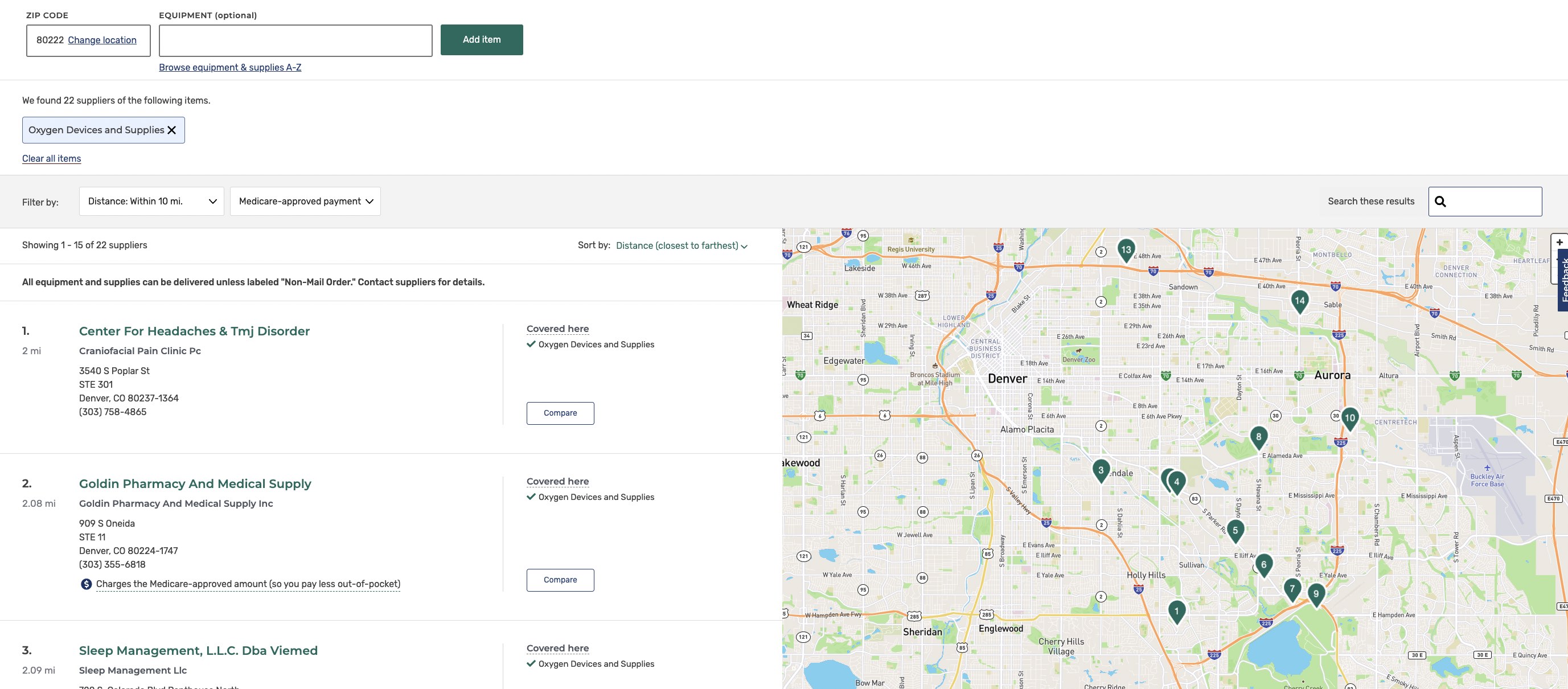
After the five-year period, if you still require oxygen supplementation, your supplier can negotiate a new five-year contract with Medicare or refuse, leaving you to find a new supplier. Finding a DME supplier to rent portable oxygen equipment from can be difficult because Medicare usually pays them the same rate whether or not it is for a stationary or portable concentrator and portable machines are more expensive. So, it makes financial sense for the DME supplier to rent you a stationary machine instead.
Some oxygen machine companies like Inogen skip the supplier and negotiate directly with Medicare themselves. They are more likely to rent you a portable machine. Finally, both your doctor and your DME supplier must be enrolled in Medicare—not all of them are. Medicare offers a supplier directory to help find Medicare-approved suppliers. Here are the results of a search in my ZIP code:
Finally, Medicare Advantage plans include Part B, so they do cover oxygen equipment but they vary in the amount of coverage. Call your provider to discuss their specific coverage plan.
When is Home Oxygen Therapy Prescribed?
According to the Annals of the American Thoracic Society, more than 1.5 million adults in the United States use supplemental oxygen for a variety of respiratory disorders to improve their quality of life and prolong survival. Home oxygen therapy is generally prescribed for anyone with hypoxemia (low blood oxygen levels) with test results suggesting that oxygen therapy would improve their oxygen levels. Hypoxia (low oxygen levels in tissues) and hypoxemia go hand in hand and may result from a number of conditions:
- Chronic Obstructive Pulmonary Disease (COPD)
- Pulmonary Fibrosis (scarring in the lungs)
- Pneumonia
- Asthma
- Sleep Apnea
- Cystic Fibrosis
- COVID-19
- Heart failure
- Sickle Cell Anemia
- Recovery from illness or surgery
- High altitude travel
- Acute respiratory distress syndrome (ARDS)
- Anemia
- Bronchitis
- Emphysema
- Pneumothorax (air in the space around your lung or collapsed lung)
- Pulmonary edema (fluid on your lungs)
- Pulmonary embolism (blood clot in your lung)
- Pulmonary hypertension (increased blood pressure in the lungs)
Hypoxia may be temporary or permanent and improving or worsening. So, in-home therapy may also be temporary or permanent and the prescription may change over time.
Hypoxia means that the organs and tissues (including the heart and brain) are not getting enough oxygen. You can imagine that this is very serious with long-term negative effects. Symptoms of hypoxia include:
- Changes in skin color, ranging from blue to red (cyanosis)
- Confusion
- Cough
- Fast heart rate (tachycardia)
- Rapid breathing
- Shortness of breath (dyspnea)
- Sweating
- Wheezing
- Headache
Regardless of the cause, chronic hypoxia has severe negative effects on the body, including shortened lifespan and should definitely be treated. NPJ Primary Care Respiratory Medicine reports that long term oxygen therapy in chronically hypoxic patients confers a significant long-term survival benefit.
Which Portable Oxygen Concentrator Brands Are Covered by Medicare?
Medicare does not determine coverage based on brand. Any brand may be covered as DME under Medicare Part B if the above described conditions are met. Brand availability will be determined by the DME supply company. Inogen is the most commonly covered brand and may be rented through a DME supplier or through Inogen directly. Other popular brands are Philips Respironics, Caire, and GCE.
Alternatives to Portable Oxygen Concentrators
Portable oxygen concentrators are one of a few ways to treat hypoxia. Before oxygen therapy is prescribed, you may try an inhaler or medication. If testing shows that oxygen therapy is necessary, it can be obtained in three ways: oxygen gas, liquid oxygen, or oxygen concentrators.
Medicare considers all forms of oxygen delivery systems durable medical equipment (DME) and covers 20% of their rental cost after your Part B deductible has been met. Because tank-based machines are less expensive, your out-of-pocket costs will be less when renting a tank-based system instead of a concentrator. Many people find that the extra expense is worth it, though, for the freedom that comes with a portable concentrator.
Bottom Line
Medicare Part B typically may cover part of the cost of renting a portable oxygen concentrator. Certain conditions must be met including evaluation and testing by a qualified medical professional and a prescription for oxygen therapy for use in the home. DME suppliers will work with Medicare to get a machine to you at a set cost for up to five years at a time. If oxygen is still required after five years, a new contract can be negotiated. Portable concentrators are more expensive than stationary concentrators or tank-based systems but many find that the freedom and mobility of a POC make the extra expense worth it.

